Liver biopsy shows protoporphyria, solving diagnostic mystery
Previously healthy 75-year-old had abdominal pain, jaundice, no skin symptoms
A liver biopsy helped doctors diagnose a 75-year-old man who arrived at the hospital with abdominal pain and jaundice (yellowing of the skin and eyes) with protoporphyria, a type of porphyria.
He recovered without treatment as his liver function improved spontaneously, according to a case report.
“This report highlights the potential role of liver biopsy in the diagnosis of protoporphyria for patients with atypical presentations,” researchers wrote in the report, “Protoporphyric Hepatopathy in a Previously Healthy Elderly Patient,” published in the International Journal of Surgical Pathology.
Protoporphyria makes the skin highly sensitive to sunlight, causing itching and burning. Its most common form, erythropoietic protoporphyria, is caused by mutations in the FECH gene. Flare-ups, or worsening of symptoms, can be triggered by many factors. Some patients, however, have no skin symptoms, which can delay their diagnosis.
In the man’s case, blood tests revealed elevated liver enzymes and bilirubin (a yellow substance that accumulates when the liver is unable to process it properly). Scans of his abdomen — ultrasound, CT, and MRI — showed no blockage or damage in his bile ducts. Because the cause of his liver problem was unclear, doctors performed a liver biopsy, a procedure in which a small tissue sample is examined under a microscope to determine the cause of an issue.
Under the microscope
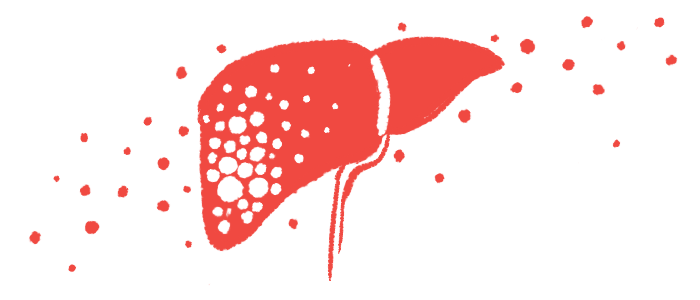
Under the microscope, the doctors found a dark-brown pigment inside liver cells and in the tiny bile channels. When viewed under polarized light, the pigment appeared red to yellow with a unique cross-like pattern. This finding is typical of protoporphyrin, confirming a diagnosis of protoporphyric hepatopathy, a condition characterized by liver damage caused by the accumulation of protoporphyrin.
The biopsy showed some mild liver scarring and inflammation, but no major cell death or fat buildup. Other tests for iron and viral hepatitis were negative, ruling out common causes of liver injury. Based on these findings, the team diagnosed the patient with protoporphyria affecting the liver.
The man had never noticed sensitivity to sunlight and declined further testing to determine whether the disease was inherited or acquired later in life. His liver tests improved without treatment, and he was discharged from the hospital.
Protoporphyria is typically diagnosed through blood tests that measure the amount of protoporphyrin in red blood cells, as well as through genetic testing. However, in this case, the diagnosis came from the liver biopsy alone. Recognizing the unique pigment pattern under the microscope was crucial for identifying the disease.
The man’s age and lack of skin symptoms made the diagnosis unusual. The liver biopsy was key to identifying the cause. It’s possible that a hidden factor, such as mild drug toxicity or infection, triggered his symptoms and revealed an underlying problem with protoporphyrin metabolism, the researchers said.
The team said the case shows how liver biopsy can aid in diagnosing protoporphyria when the disease is not initially suspected. Recognizing the distinctive pigment in liver tissue is essential for correct diagnosis and management. Further genetic or bone marrow testing would have helped confirm whether the man’s condition was inherited or acquired later in life, the researchers said.