Bioenergetic Tests May be Useful Biomarkers of Porphyria Activity, Study Says
Non-invasive bioenergetic tests may be useful biomarkers to assess disease activity in patients with different types of porphyria, a study says.
The study, “Feasibility of cellular bioenergetics as a biomarker in porphyria patients,” was published in Molecular Genetics and Metabolism Reports.
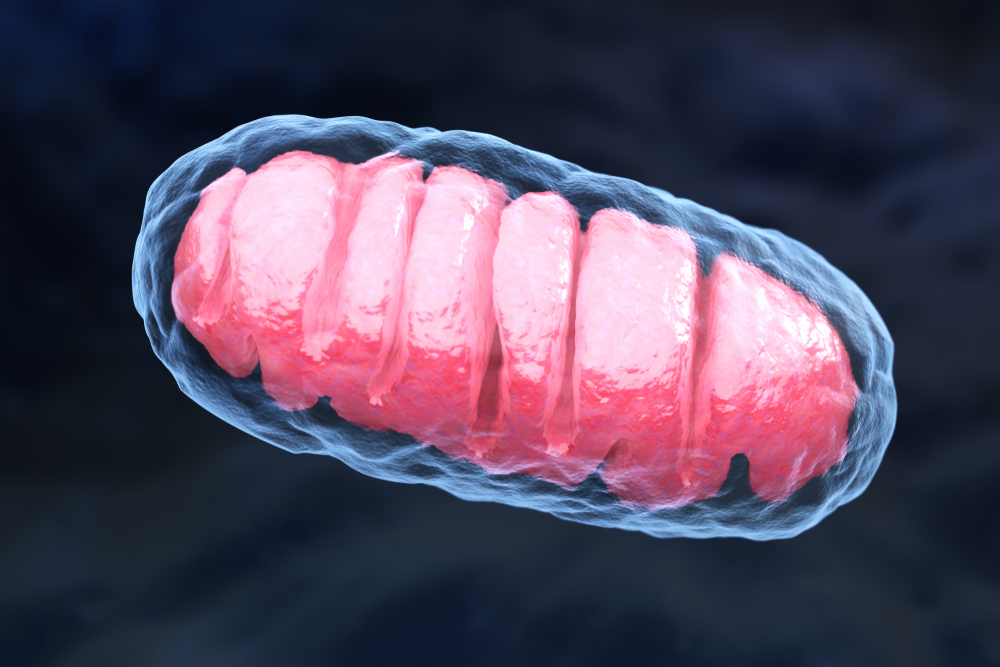
Porphyrias are a group of genetic metabolic disorders characterized by the body’s inability to produce heme — a molecule essential for red blood cells’ oxygen transport and compounds’ breakdown in the liver. It is a systemic disorder that has also been associated with mitochondrial dysfunction and oxidative stress.
Mitochondria are the the cell compartments responsible for the production of energy. When mitochondria malfunction, cells are unable to produce enough energy to sustain their normal activity, which may lead to health problems. Oxidative stress refers to the cellular damage that occurs as a consequence of high levels of oxidant molecules.
“It has been shown that circulating blood cells interact with various tissues and organs, and the mitochondrial health and bioenergetics of peripheral blood cells are a direct reflection of the disease state [in several disorders, including] diabetes mellitus, sepsis, neurodegenerative diseases, and alcoholic liver disease …” the investigators said.
In this study, a group of researchers from the University of Alabama set out to examine whether mytochondria dysfunction and cell bioenergetics might also play a role in porphyria.
Investigators isolated peripheral blood cells from a group of 22 adult patients with porphyria — 12 with porphyria cutanea tarda (PCT), seven with acute hepatic porphyria (AHP), and three with erythropoietic protoporphyria (EPP) — and 18 age- and sex-matched healthy individuals.
They performed a battery of lab tests to examine the participants’ bioenergetic profiles. These tests included cells’ oxygen consumption rate (OCR) at normal conditions, adenosine triphosphate (ATP) production, maximal and reserve capacity. ATP is a molecule produced by mitochondria that is used as a source of energy, or fuel, by all cell types in the body. The maximal and reserve capacity refer to the peak and stored backup energy produced by cells.
Among patients with porphyria, eight had active disease and 14 were in biochemical remission.
Bioenergetic analyses revealed the OCR was lower among patients with porphyria, compared to healthy controls. In addition, the overall bioenergetic profile of peripheral blood cells isolated from patients with active porphyria was significantly lower compared to that of healthy individuals.
“[Our] novel preliminary findings suggest the existence of a mitochondrial dysfunction in porphyria and this may be used as potential non-invasive biomarker for disease activity. This needs to be assessed with a systematic examination in a larger patient cohort,” the scientists said.
“Further, mechanistic studies are also needed using mitochondrial metabolomics as an approach to localize the defects in mitochondria, as basis for developing therapeutic targets and newer mitochondrial based therapies for patients with porphyria,” they concluded.






