Delay in AIP diagnosis shows how it can be misdiagnosed in early stages
Patient first diagnosed with PRES, a rare condition marked by brain swelling
Written by |
A 26-year-old man who developed seizures, muscle weakness, and abdominal pain was eventually diagnosed with acute intermittent porphyria (AIP), a Chinese study reports.
The patient was initially diagnosed with posterior reversible encephalopathy syndrome (PRES), a rare condition marked by swelling in the brain, but a biochemical and genetic analysis later confirmed AIP.
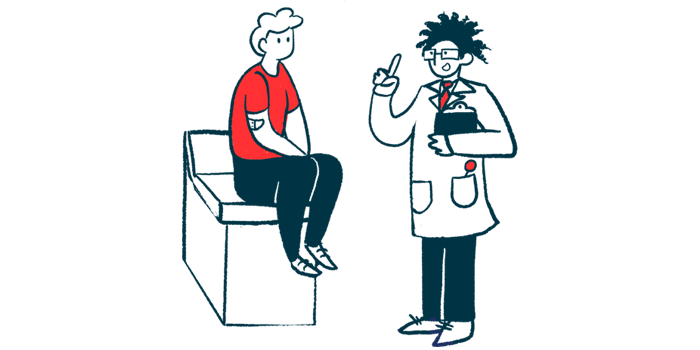
“When a patient presents with … nervous system symptoms and common causes are ruled out, AIP should be considered as a potential diagnosis. Additionally, unexplained symptoms such as abdominal pain, changes in urine color, hyponatremia [low blood sodium levels] should also raise suspicion,” the researchers wrote.
The report “An easily overlooked disease in the early stages: acute intermittent porphyria,” was published in BMC Neurology.
AIP, the most common form of acute porphyria, is caused by mutations in the HMBS gene. Like other forms of porphyria, it’s marked by the toxic buildup of heme precursors. In AIP, sudden attacks occur, which may be triggered by an infection or hormonal changes.
Common AIP symptoms include abdominal pain and neurological dysfunction, which can manifest in the form of seizures, confusion, and altered mental status. Because abdominal pain overlaps with other diseases, it’s often overlooked, which can delay an AIP diagnosis.
Difficulty of early AIP diagnosis
Here, the man sought medical attention due to seizures. His medical history showed that five months earlier, he’d had severe abdominal pain on his right side, dark-colored urine, and frequent vomiting. At the time, clinicians suspected a urinary tract infection and his symptoms eased after treatment. A month before his hospital admission, however, he had two major seizures, along with excessive sweating, and repeated vomiting.
When he arrived at the hospital, tests showed high blood pressure, an unusually fast heart rate, and low sodium. A brain MRI scan revealed abnormalities, leading to a diagnosis of PRES. He was given medications to lower his blood pressure, prevent seizures, and control nausea and vomiting and no more seizures occurred, but the man later noticed he was unable to lift his arms above his shoulders.
When a patient presents with … nervous system symptoms and common causes are ruled out, AIP should be considered as a potential diagnosis. Additionally, unexplained symptoms such as abdominal pain, changes in urine color, hyponatremia should also raise suspicion
A follow-up MRI scan showed that some of his brain abnormalities still remained.
Physicians initially suspected Guillain-Barré syndrome, a condition wherein the immune system mistakenly attacks nerves, but his condition didn’t improve after five days of antibody-based therapy.
Ten days into his hospital stay, the man’s symptoms worsened. He started having severe limb pain, constipation, bloating, and abdominal pain. His arm weakness spread to his hands, making it difficult to hold objects. These symptoms along with further testing pointed toward AIP as the cause of his illness.
Easily overlooked
Without immediate access to hemin, the man’s condition continued to deteriorate. His muscle weakness progressed and he lost the ability to sit, stand, or even swallow properly. He also began having psychiatric symptoms, including hallucinations and delusions.
He was started on carbohydrate therapy, due to a lack of hemin, and a subsequent biochemical and genetic test confirmed the AIP diagnosis. Five weeks after being admitted, he was started on heme arginate, a medication sold under the brand name Normosang and commonly used as a first-line treatment for severe porphyria attacks. He also continued to receive carbohydrate therapy.
Within eight days of starting treatment, his urine color returned to normal, and his digestive and psychiatric symptoms resolved.
The man’s condition slowly improved over two months and he was able to walk slowly with assistance.
Three months after his admission, he likely had another porphyria attack, with severe muscle and abdominal pain, nausea, and red-colored urine. Another round of hemin infusions helped him recover. After four and a half months, he could walk independently for several hundred meters and move his arm in a circular motion. The man still struggles with wrist drop and has difficulty straightening his fingers.
“This case unveils that AIP is a disease that can be easily overlooked in its early stages,” the researchers wrote. However, “timely administration of intravenous [into-the-vein] hemin and avoidance of precipitating factors can lead to a better prognosis.”