Researchers report first documented case of mosaic mutation in AIP
Mutation affected only a fraction of man's cells in rare case
Written by |
Scientists in Switzerland have reported the first documented case of acute intermittent porphyria (AIP) caused by a mosaic mutation — a genetic mutation that affected only a fraction of the patient’s cells.
Their findings suggest that new mosaic mutations could potentially be the cause for acute porphyria in other rare cases.
“To our knowledge, such a mutation has not been previously described in any acute porphyria,” the scientists wrote. “Therefore, de novo [not inherited] mosaic mutations should be considered as potential causes of acute porphyrias when no pathogenic [disease-causing] genetic variant can be identified through routine molecular diagnostics.”
The study, “First Report of a Low-Frequency Mosaic Mutation in the Hydroxymethylbilane Synthase Gene Causing Acute Intermittent Porphyria,” was published in Life.
First documented case details not-inherited genetic mutation
AIP is caused by mutations in the gene HMBS, which provides instructions for making a protein with the same name. Like other types of porphyria, AIP is marked by the toxic buildup of molecules called porphyrins, which drives disease symptoms.
In this study, scientists described the case of a man who was diagnosed with AIP in 2017 following an acute attack that required intensive medical care. His symptoms included abdominal pain, nausea, constipation, abnormal blood pressure, and confusion.
The attack occurred following a viral infection, during which the patient received treatment with mefenamic acid and metamizole — two drugs known to be able to trigger porphyria attacks.
The patient said he had never experienced such an attack before, and to his knowledge, there was no history of porphyria in his family.
The man was diagnosed with AIP based on his symptoms, combined with laboratory tests results, such as findings of elevated porphyrins in the urine. Following the diagnosis, he underwent testing to look for a disease-causing mutation.
An initial test that assesses most of the protein-coding parts of the HMBS gene did not show any abnormalities. Tests of the patient’s blood showed that HMBS protein activity was slightly lower than normal, by about 12%.
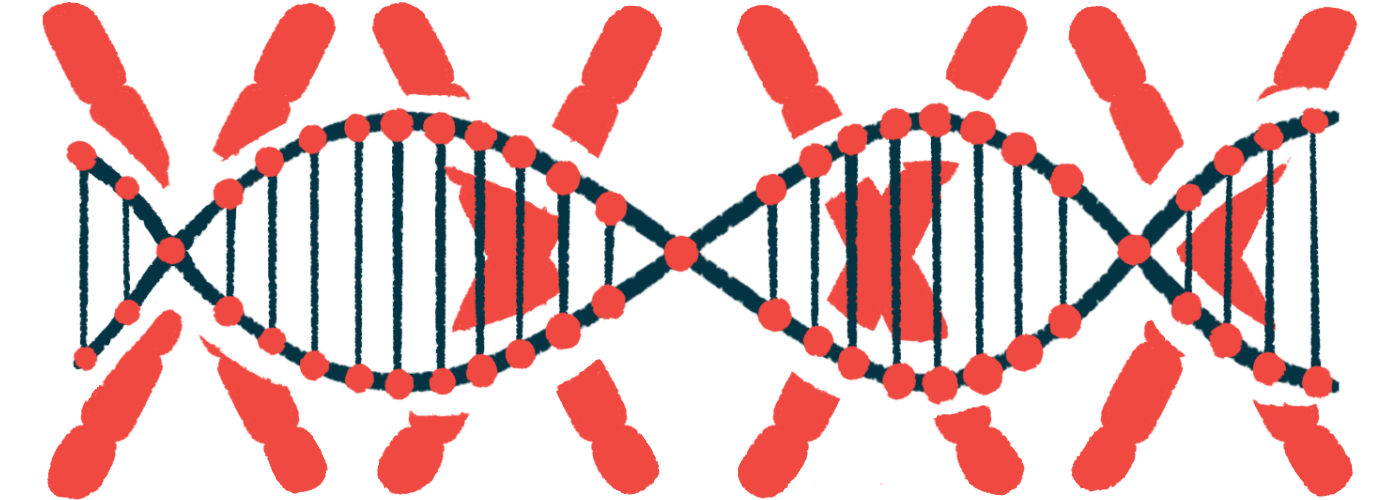
Following these ambiguous results, the patient underwent nanopore sequencing, which is a recent technology that can determine the sequence of genes in greater detail than older methods of genetic sequencing. This more advanced test showed a known disease-causing mutation in HMBS called c.77G>A — but the mutation was only present in about a fifth of the man’s blood cells.
This represents an example of a genetic phenomenon called mosaicism, where some of a person’s cells have a mutation that isn’t present in the rest of the person’s cells — a bit like differently colored tiles being put together to form a mosaic, which is how the term gets its name.
Because symptoms of AIP are driven by reduced HMBS activity in the liver, the researchers speculated that the mutation might be particularly common in this patient’s liver cells. However, as taking samples of the liver would be invasive, this idea has not been tested.
Testing of the man’s parents showed that neither of them carried this mutation, suggesting that it developed de novo. In other words, the mutation occurred for the first time in the man, rather than being inherited from his parents.
Importantly, though, the mutation was present in some of the man’s sperm cells, meaning it is possible he could pass it on to his biological children.
This is the first time that a de novo mosaic mutation has been documented to cause AIP, the researchers said.