New AIP-causing HMBS gene mutation ID’d in woman
Researchers say genetic testing crucial in diagnosing AIP in those asymptomatic
Written by |
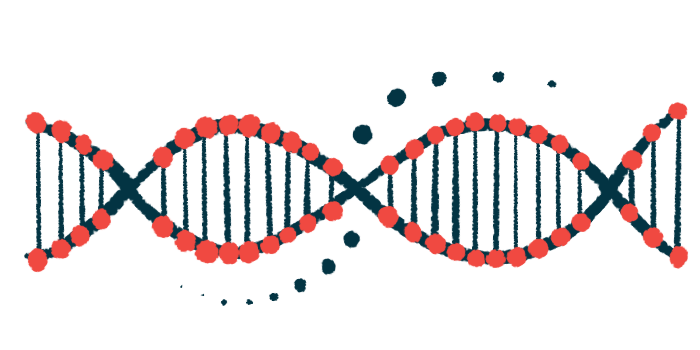
A new mutation in the HMBS gene was identified as the cause of acute intermittent porphyria (AIP) in a woman, and also detected in her daughter, who showed no symptoms of the disease, according to a study in China.
The mutation was found to affect splicing — the process by which parts of a gene can be cut and joined together in different combinations — leading to the production of two faulty versions of the HMBS enzyme.
“This finding not only expands the molecular heterogeneity [diversity] of AIP but also provides crucial information for genetic diagnosis,” researchers wrote. That can be important for people who carry disease-causing mutations but haven’t yet shown symptoms.
The study, “Genetic analysis of acute intermittent porphyria caused by novel classical splicing variant in the insertion region of 29-residue specific to human HMBS protein,” was published in Frontiers in Molecular Biosciences.
The most common of acute porphyrias, AIP is caused by mutations in HMBS, a gene that codes for an enzyme known as hydroxymethylbilane synthase or HMBS. This enzyme is responsible for the third of eight steps to make heme, a key component of many proteins.
There are hundreds of known mutations in HMBS, which can change, add, or delete genetic material within the gene, altering the enzyme’s shape and function.
Some mutations affect splicing, the process by which a gene can give rise to different proteins by joining exons in different combinations. An exon is a protein-coding region of a gene.
Now, researchers in China identified a disease-causing mutation in one of the copies of the HMBS gene in a woman who “had previously received treatment for sudden general paralysis and was diagnosed with AIP,” the researchers wrote.
Symptoms of acute porphyrias emerge suddenly and may include pain in the abdomen or in other parts of the body, paralysis, constipation or vomiting, and changes in mental status.
Seeking cause of AIP leads to find of previously unreported mutation
To find the cause of AIP, the researchers scanned through all the exons in the woman’s genome. They identified a mutation, called c.912 + 1G>C, in intron 13 of one of the copies of the HMBS gene. The other copy was wild-type (normal). An intron is a noncoding region that’s usually cut out before a protein is made.
The mutation, also detected in the woman’s daughter, “has not been previously reported in scientific literature,” the researchers wrote.
More detailed analysis revealed that as a result of the splicing error, the messenger RNA derived from the HMBS gene — a template from which a protein is made — retained intron 13 and skipped over exon 13 which was 87 building blocks too short.
The resulting enzymes were shorter and less stable than the wild-type HMBS. Computer modeling revealed that these enzymes may not be active. The mutation “can lead to a complete loss of enzyme activity,” the researchers wrote.
Besides the two faulty versions of the enzyme, the researchers also detected the wild-type mRNA, and at higher levels. This suggests that the wild-type HMBS “plays a dominant role in [the] patient, which may indicate that the symptoms are not severe.”
The levels of porphyrins, which are normally used to make heme, can be measured in urine or blood. However, people who are asymptomatic, or haven’t yet shown symptoms, may not have high levels of porphyrins.
“Hence, genetic testing is crucial in diagnosing AIP in asymptomatic patients,” the researchers wrote. “When conducting family screening for AIP patients, there is a good chance that other family members may have the same mutation.”
With this information in hand, people who carry disease-causing mutations may be able to avoid the triggers typically needed to set off symptoms of the disease, the scientists noted.