New treatment prevents light-induced skin damage in EPP mice
Scientists testing oral therapy to block ABCG2 protein in red blood cells
Written by |

A newly developed treatment to prevent phototoxicity, or light-induced skin damage, was found effective in a mouse model of erythropoietic protoporphyria (EPP), a common form of porphyria marked by skin hypersensitivity to sunlight and some types of artificial light, a study showed.
The novel oral therapy is designed to block ABCG2, a transporter protein in red blood cells that’s linked to phototoxicity.
In this study, the treatment’s use in a mouse model of EPP prevented damage to skin layers in animals exposed to light, according to the researchers.
“Our results revealed that oral ABCG2 inhibitors can effectively prevent phototoxicity in EPP,” the scientists wrote, adding that “this ABCG2-inhibiting approach is mechanistically different from the currently available methods used for preventing EPP-associated phototoxicity.”
The study, “Inhibition of ABCG2 prevents phototoxicity in a mouse model of erythropoietic protoporphyria,” was published in Nature Communications.
Researchers create treatment strategy based on findings of 2019 study
Porphyria is a group of rare genetic diseases marked by an impaired production of heme, a molecule that helps transport oxygen in red blood cells. As a result, heme precursors, called porphyrins, build up in different tissues and organs, eventually reaching toxic levels.
EPP, the most common childhood porphyria, is caused by mutations in the FECH gene, which encodes an enzyme called ferrochelatase. Without this enzyme, protoporphyrin IX, or PPIX, builds up in the skin, blood, and liver, leading to extreme sensitivity to sunlight — known as phototoxicity, it’s EPP’s hallmark symptom.
PPIX is mainly produced in the bone marrow and released from red blood cells into the bloodstream via a transporter protein called ABCG2. Excess PPIX then moves into the skin and causes phototoxicity when it’s excited by sunlight.
In 2019, a team led by researchers at the University of Pittsburgh in Pennsylvania, showed that an EPP mouse model lacking ABCG2 was protected from light-induced skin blisters.
Now, these scientists have developed an orally available ABCG2 inhibitor and set out to test it in EPP mice. Their goal: To investigate the “therapeutic potential of ABCG2 inhibitors against EPP-associated phototoxicity.”
Specifically being tested was K31, a modified version of Ko143, a classic ABCG2 inhibitor. Compared with its predecessor, K31 was more stable, less toxic, and readily absorbed into the bloodstream after oral dosing.
After shaving back the animals’ hair to expose the skin, male and female EPP mice were pretreated orally with K31, and then exposed to light for 20 minutes. This was repeated once daily for five days.
Novel treatment found to prevent skin damage from phototoxicity
In EPP mice treated with K31, light-triggered phototoxicity was significantly attenuated in both sexes, as indicated by the overall appearance of the skin. Under a microscope, damage to the skin layers seen in untreated mice was prevented with K31 treatment. Moreover, EPP mice treated with K31 had reduced signs of inflammation and oxidative stress, a type of cellular damage resulting from an imbalance between oxidative and antioxidant molecules.
However, when K31 treatment was stopped, light-triggered phototoxicity recurred, “indicating the ABCG2 inhibitor-dependent effect against EPP-associated phototoxicity,” the team wrote.
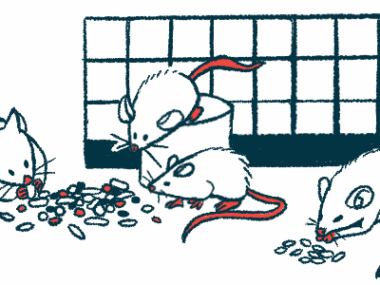
Similar to the results seen with EPP mice lacking ABCG2 in the earlier study, K31 also blocked the release of PPIX from red blood cells. This was found to significantly lower the levels of PPIX in the blood of treated EPP mice.
The current work has established a novel strategy against EPP-associated phototoxicity by inhibiting ABCG2. … Our work could fill a therapeutic gap in EPP by providing oral ABCG2 inhibitors for preventing [skin damage].
In safety studies, five days of K31 treatment had no significant impact on red blood cells, the liver, or kidneys in EPP mice or healthy mice.
“The current work has established a novel strategy against EPP-associated phototoxicity by inhibiting ABCG2,” the researchers wrote.
The team noted that these findings show the potential benefits of a treatment blocking this protein.
“Our work could fill a therapeutic gap in EPP by providing oral ABCG2 inhibitors for preventing PPIX-mediated phototoxicity,” the researchers wrote.