Rare dual diagnosis of lupus and PCT detailed in case report
Co-occurrence of disorders presents treatment challenges for physicians
Written by |

A recent case report describes a rare instance of a woman diagnosed with both porphyria cutanea tarda (PCT) and systemic lupus erythematosus (SLE), an autoimmune disease. Her diagnosis was confirmed through laboratory tests and tissue biopsies.
“The diagnosis of both pathologies becomes a challenge for physicians in diagnosis and treatment, as shown in this case, since porphyria can be the first and only manifestation of underlying systemic lupus erythematosus,” researchers wrote.
The case was described in a report, titled “Porphyria cutanea tarda and systemic lupus erythematosus: a case report.” It was published in the Journal of Medical Case Reports.
Lab work, skin biopsy led to diagnosis of lupus and PCT
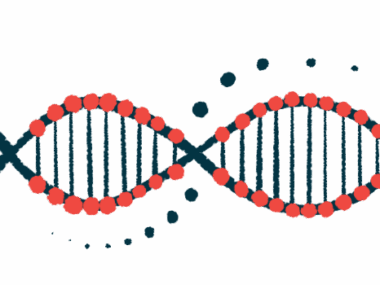
Porphyria is a group of genetic disorders caused by problems in making heme, an important molecule in the body. When this process gets disrupted, substances called porphyrins build up, mainly in the skin and liver. Heme is made of iron and another part called protoporphyrin IX, and it helps red blood cells carry oxygen.
PCT, the most common type of porphyria, is caused by low levels of an enzyme called uroporphyrinogen decarboxylase, which helps the body produce heme. It is characterized by sunlight sensitivity that leads to the formation of painful skin lesions and blistering in sun-exposed areas. Liver involvement is also common in people with PCT.
In this report, researchers in Colombia described the case of a 62-year-old woman who presented with an eight-month history of skin lesions on the hands, fingers, forearms, and right foot and ankle. Upon physical examination, she had skin darkening and excessive hair growth in areas exposed to sunlight, particularly on the face.
She was taking immunosuppressive medications due to a history of kidney transplantation due to previous kidney disease associated with diabetes.
During hospitalization, changes in urine color upon sunlight exposure were detected, and laboratory work indicated she had elevated levels of iron and ferritin – a protein that stores iron within cells – and of uroporphyrins in the urine. This, together with the patient’s symptoms and a skin biopsy, led to a diagnosis of cutaneous porphyria.
Further analysis found antinuclear antibodies (ANAs), which attach to parts inside the cell’s nucleus where DNA is kept. Some of these antibodies target double-stranded DNA (dsDNA), an indicator of SLE, the most common type of lupus, an autoimmune disease that can affect many parts of the body.
Disorders are rarely found together in one patient
The woman began treatment with an antimalarial therapy called hydroxychloroquine, which has been used to reduce lupus inflammation and to help treat PCT. However, she experienced an elevation of liver enzymes that led to treatment suspension after three days, which resolved the liver alteration.
Further abdominal MRI scans revealed the woman’s liver was enlarged and had excess fat buildup. A liver biopsy showed iron accumulation and inflammation in the liver. The researchers restarted hydroxychloroquine treatment at lower doses, closely monitoring her liver function, which led to a positive response.
These combinations establish a diagnostic and therapeutic challenge, which impacts organ damage or dysfunction, prognosis, and mortality for patients.
According to the team, 13 articles have described cases of PCT and systemic lupus. Most patients were women with an average age of 40 years who mainly had skin darkening and hair growth in sunlight-exposed areas, as well as skin blisters.
They typically tested positive for ANAs and anti-dsDNA antibodies and were primarily treated with low-dose antimalarial drugs, sometimes combined with corticosteroids. Treatment also included protection from sunlight and blood removal, or phlebotomy, a procedure that reduces levels of certain harmful substances by removing a controlled amount of blood.
“These combinations establish a diagnostic and therapeutic challenge, which impacts organ damage or dysfunction, prognosis, and mortality for patients,” the researchers wrote. They added “there is still a lack of data that define whether the presentation of these two [conditions] is a true combination of diseases, an autoimmune or immunological epiphenomenon, or a shared genetic development.”