New trial results show bitopertin eases a major driver of EPP symptoms
Treatment lowered PPIX and supports further study of bitopertin in EPP
Written by |
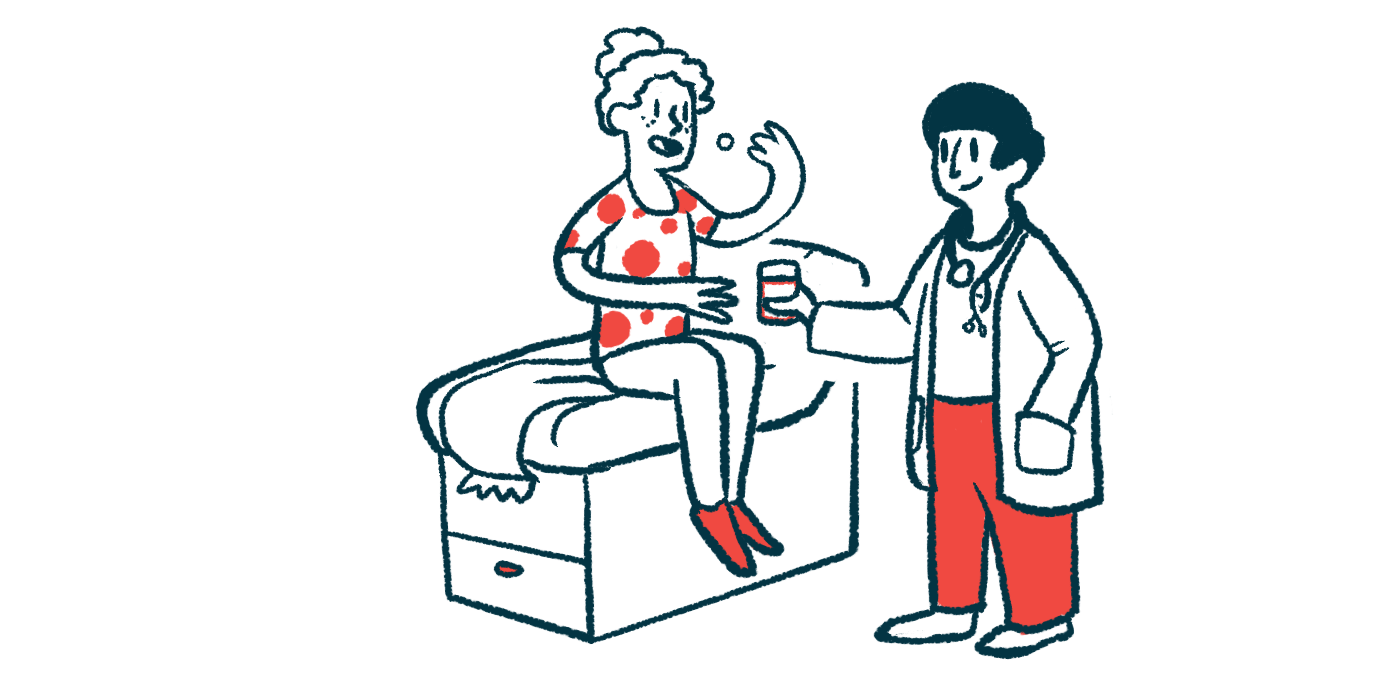
Treatment with the investigational oral therapy bitopertin significantly reduced protoporphyrin-IX (PPIX) levels and was generally well tolerated in adults with erythropoietic protoporphyria (EPP), meeting the main goal of the Phase 2 AURORA clinical trial.
Because toxic PPIX buildup is a major driver of EPP symptoms, the reductions seen in AURORA were accompanied by fewer painful reactions to sunlight and improvements in patient-reported disease severity. Additional analyses also suggested gains in pain-free sunlight tolerance, particularly after about seven weeks of treatment.
“These results support [bitopertin] continued development as a treatment option for erythropoietic protoporphyria, a debilitating disorder with no approved disease-modifying therapies,” the researchers wrote.
Bitopertin targets a key buildup behind EPP’s painful light reactions
The study, “Bitopertin shows efficacy in patients with erythropoietic protoporphyria: Results from the randomized, double-blind, placebo-controlled AURORA trial,” was published in the Journal of the American Academy of Dermatology. The trial was sponsored by Disc Medicine, the company developing bitopertin.
Like other types of porphyria, EPP is caused by a problem in the body’s ability to make heme, a molecule needed to carry oxygen in the blood. When heme production is disrupted, building blocks along the pathway, including PPIX, can accumulate, mainly in red blood cells.
When exposed to certain wavelengths of light, accumulated PPIX can generate reactive oxygen species, triggering early symptoms such as skin burning, itching, and tingling. These symptoms can worsen into phototoxic reactions, with intense burning pain, swelling, and erythema (skin redness) that may last for days. EPP is also linked to a higher risk of liver complications.
Bitopertin targets glycine transporter 1 (GlyT1), a protein that helps deliver glycine — a key building block used early in heme production — to red blood cells. By reducing glycine availability, bitopertin is designed to lower downstream PPIX formation, which may help ease symptoms and improve tolerance to sunlight.
Bitopertin was previously studied in adults with EPP in the Phase 2 BEACON clinical trial (ACTRN12622000799752). That study reported increased time in the sun, though it did not include a placebo group for comparison.
Phase 2 AURORA trial tests two daily doses against placebo
To further evaluate bitopertin, the AURORA trial (NCT05308472) enrolled 75 adults with EPP at nine U.S. centers between December 2022 and October 2023. Participants were randomly assigned to receive once-daily oral bitopertin at 20 mg or 60 mg, or a placebo, for 17 weeks, or about four months of treatment.
Roughly half of the participants were female, and the average age was in the mid-40s. The three groups were generally similar in age and sex. All participants started with markedly elevated blood PPIX levels, and the higher-dose group had numerically higher baseline PPIX levels and slightly lower baseline light tolerance than the other groups. Seventy-two participants (96%) completed the study.
The trial’s primary goal was to measure changes in PPIX levels. Secondary endpoints included sunlight sensitivity and treatment tolerability.
These results support [bitopertin] continued development as a treatment option for erythropoietic protoporphyria, a debilitating disorder with no approved disease-modifying therapies.
Consistent with previously reported top-line results, patients receiving bitopertin showed significant, dose-dependent reductions in PPIX levels compared with placebo. By the end of the study, PPIX levels increased by 8.1% in the placebo group. Compared with placebo, bitopertin was associated with greater reductions in PPIX levels: an estimated 29.6% more with the 20 mg dose and 49.8% more with the 60 mg dose.
PPIX levels reached their lowest point after about seven weeks of treatment and remained stable through the end of the study. These reductions were consistent across subgroups, including age, sex, baseline PPIX levels, and baseline light tolerance.
Although the study’s key secondary sunlight endpoint did not differ significantly between groups overall, a post hoc analysis using two-week intervals suggested pain-free sunlight time increased with bitopertin and became more pronounced after about seven weeks, when PPIX levels reached their lowest point.
Higher dose linked to longer pain-free sunlight time in added analyses
By the end of the study, patients receiving 60 mg averaged 21.7 hours of pain-free sunlight exposure over a two-week period — about twice as much as before treatment — and this was significantly longer than in the placebo group.
Phototoxic reactions were also less frequent with bitopertin. During the final 60 days of treatment, no patients in the 60 mg group experienced painful reactions to sunlight, compared with 4% in the 20 mg group and 38% in the placebo group.
Improvements in patient-reported EPP severity were more common among patients treated with bitopertin. By the end of the study, 85% of patients receiving 20 mg and 86% of those receiving 60 mg reported their EPP was “much better” or “a little better,” compared with 67% in the placebo group.
Improvements in pain-free sunlight exposure, fewer phototoxic reactions, and better quality-of-life measures were most pronounced among patients who had the largest reductions in PPIX levels.
Bitopertin was generally well tolerated. Most side effects were mild to moderate, and dizziness was the most frequently reported. No serious adverse events were reported in the bitopertin groups. Two participants in the 60 mg group discontinued treatment due to side effects (dizziness and rash), and one participant discontinued due to iron deficiency anemia that began before treatment. One serious adverse event occurred in the placebo group.
The researchers wrote that the AURORA results support the continued development of bitopertin for EPP, “offering new therapeutic promise for a patient population with historically limited options.”
They noted that the study’s relatively small size and short duration were limitations and wrote that additional studies are needed to clarify bitopertin’s impact on the risk and progression of liver complications.