Variegate porphyria skin fragility worsens sun damage, study shows
Impaired formation of protective layers raises vulnerability
Written by |
Skin damage in variegate porphyria (VP) is worsened by impaired formation of the protective outer skin layers, according to a study using skin cells.
The study, “Reduced PPOX expression causes intrinsic pathogenicity in keratinocytes, contributing to the cutaneous Variegate Porphyria phenotype,” was published in the Journal of Investigative Dermatology.
In porphyria, genetic mutations result in a deficiency of enzymes necessary for the production of heme, the iron-containing molecule in red blood cells that facilitates oxygen transport through the body. When heme production is disrupted, heme precursors, known as porphyrins, rise to toxic levels, leading to disease symptoms.
VP is a type of porphyria caused by mutations in one copy of the PPOX gene — and in rare cases, both gene copies — which reduces the production of the enzyme protoporphyrinogen oxidase. This results in the accumulation of porphyrins, including those derived from aminolevulinic acid, or ALA. When these porphyrins build up near the skin, sunlight activates them, causing painful blistering and fragile skin.
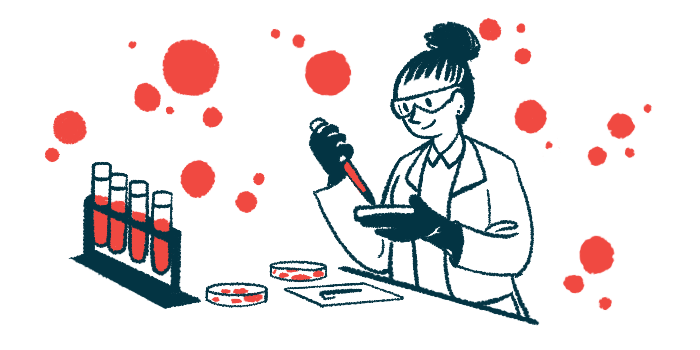
A team at Queen Mary University of London investigated whether reduced PPOX activity in skin cells known as keratinocytes contributes to skin problems in VP, in addition to the damage caused by porphyrin buildup from sunlight exposure.
Cell experiments lead researchers to propose ‘updated paradigm’
The researchers created two keratinocyte cell lines in which the activity of one (KD1) or both (KD2) PPOX gene copies was suppressed to mimic VP in the skin. Residual enzyme production was reduced to 52% of normal in KD1 cells and to 23% in KD2 cells.
Experiments demonstrated that proliferation, the process of increasing cell numbers through cell growth and division, was significantly reduced in both KD1 and KD2 keratinocytes. Migration, the movement of cells to a new location, was significantly impaired in KD2 cells, which have more suppressed enzyme production.
While heme is primarily produced in the bone marrow and the liver, the team confirmed that keratinocytes also have a heme synthetic pathway.
Keratinocytes arise, or differentiate, from stem cells, which then migrate towards the skin surface to become corneocytes, the cells that make up the outermost layer of the skin. Tests showed that, in addition to porphyrin accumulation, low PPOX activity levels significantly affected keratinocyte differentiation.
To closely mimic actual skin layers, the team followed keratinocyte differentiation in 3D organoids, tiny, lab-grown versions of real organs. Similar to individual cells, the differentiation of KD2 cells was impaired in the organoids, leading to a thinner skin layer. When the researchers added a type of ALA, known as 5-ALA, keratinocyte differentiation was further affected, impairing the cells’ ability to form a normal skin layer.
“We propose an updated paradigm of porphyria skin manifestations: porphyrin excitation beneath the skin is facilitated by a thinner, less differentiated barrier,” the team wrote.
Porphyrin buildup, achieved by treating keratinocytes with 5-ALA and a molecule that binds iron (deferoxamine), also triggered signs of oxidative stress — a type of damage caused by an excess of reactive oxygen species over the antioxidants that neutralize them.
“Here we have shown that reduced PPOX [activity] in keratinocytes negatively impacts their proliferation and differentiation and enhances their accumulation of porphyrin intermediates,” the researchers wrote.