AIP nerve damage symptoms may result in misdiagnosis: Case report
Woman, 41, was initially believed to have Parsonage-Turner syndrome
Written by |
Note: This story was updated Nov. 4, 2024, to correct that Givlaari was given via subcutaneous injections, not through infusions.
Upper body pain and muscle weakness led to a misdiagnosis of Parsonage-Turner syndrome (PTS) for a woman in France who was later found to have acute intermittent porphyria (AIP), a case study reports.
While PTS, which causes similar nerve damage-related symptoms, typically resolves on its own, and the woman did show some improvement after her diagnosis, her motor weakness worsened after about a year and was accompanied by abdominal pain and severe constipation. Biochemical and genetic testing confirmed an AIP diagnosis.
“This case underscores the need to consider AIP in the differential diagnosis of acute [nerve damage-related conditions] like [PTS], especially when accompanied by abdominal pain and severe constipation,” the researchers wrote.
The case study, “Neuralgic amyotrophy presentation of acute intermittent porphyria: A case report,” was published in the Journal of the Peripheral Nervous System.
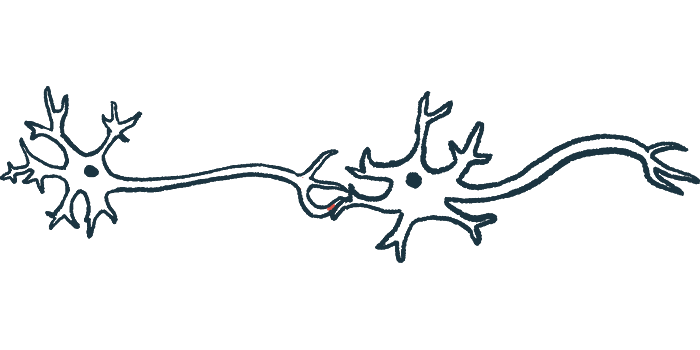
AIP, the most common form of acute porphyria, is caused by mutations in the HMBS gene that result in a deficiency of an enzyme involved in producing heme, a compound needed for red blood cells to carry oxygen. Without the enzyme, heme precursors such as porphobilinogen (PBG) and delta-aminolevulinic acid (ALA) accumulate to toxic levels in tissues, causing several symptoms.
AIP symptoms typically include intermittent attacks of pain, most commonly in the abdomen, but also in other parts of the body, such as the neck, arms, or legs. Gastrointestinal symptoms are also common, and patients can have numbness or tingling, pain, and muscle weakness as a result of peripheral neuropathy, that is, damage to the nerves outside the brain and spinal cord. The symptoms overlap with many other diseases, making a diagnosis challenging.
An initial misdiagnosis of PTS
The woman, 41, was first admitted to the emergency room with fatigue, weight loss, headache, hearing abnormalities, and shortness of breath that lasted several weeks. Swallowing was painful for her and was treated with antibiotics, because it was believed to be caused by an infection. She had a history of fibromyalgia, or widespread muscle pain, and used cannabis.
Blood testing revealed severe anemia, or low numbers of red blood cells, for which she received blood transfusions. During a two-week hospital stay, she developed pain that was particularly severe in the abdomen, which doctors thought was a symptom of cannabis withdrawal.
About a month later, the woman returned due to worsening pain in her shoulder and trunk “characterized by severe shock-like and burning sensations, present both at rest and during sleep,” the researchers wrote. The pain had rapidly progressed to muscle weakness in the shoulders, arm, and fingers, which was confirmed with clinical examination.
Specialized tests revealed problems in the brachial plexus, a network of nerve fibers that send motor and sensory signals from the spinal cord to the shoulders, arms, and hands. The muscles supplied by the nerves were also affected.
The doctors diagnosed her with Parsonage-Turner syndrome, or neuralgic amyotrophy, an uncommon disease marked by sudden pain in the shoulder and upper arm, followed by muscle weakness, due to damage to the brachial plexus. Supporting the diagnosis was the fact that the woman “was treated for an infection a few weeks before the neurological symptoms, as observed in almost half of the patients with [PTS],” the researchers wrote.
The disease usually goes away on its own, so no disease-specific treatment was prescribed. The woman’s symptoms diminished in the following months, but she had an acute relapse a little over a year after the onset of her condition, namely worsening muscle weakness in her left hand, along with burning pain in her abdominal area and severe constipation for two weeks. She received opioids for pain relief, but had hallucinations for two days.
Tests confirm AIP diagnosis
Two months later, she showed severe weakness in her left finger and signs of nerve damage worsening on specialized tests. Due to these symptoms atypical of PTS, the doctors tested her urine, which was orange in color. It showed high levels of PBG and ALA, and genetic testing identified a known disease-causing mutation in the HMBS gene, confirming a diagnosis of AIP.
The woman was treated for four days with hemin, which the body can use to produce heme, to manage her acute symptoms. To prevent them from returning, she also received Givlaari (givosiran), which was stopped after two monthly subcutaneous, or under-the-skin, injections because her symptoms had eased. She remained stable five months after the last injection.
“Clinicians should consider the diagnosis of AIP and use … urine testing for PBG and ALA levels when encountering a patient presenting with [a PTS profile] associated with abdominal pain, severe constipation, neuropsychiatric symptoms … especially if relapses occur,” the researchers wrote. “Early recognition and appropriate testing for PBG and ALA can prevent misdiagnosis and enable targeted treatment.”